Gum disease is a common problem that affects millions of people, but many wonder, can you only have gingivitis in one tooth. While most cases involve multiple teeth, it is possible for localized gingivitis to develop around a single tooth. This often happens when plaque buildup accumulates in hard-to-clean areas, or when dental issues like crooked teeth or poorly fitted crowns irritate the gums. People may notice bleeding gums, redness, or tenderness near the affected tooth. Understanding how single-tooth gum disease develops, its symptoms, and proper care is crucial. Early treatment can prevent it from spreading and causing more serious dental problems.
Gingivitis is one of the most common oral health issues, but many people wonder, can you only have gingivitis in one tooth. Most individuals assume that gum disease affects the entire mouth, yet there are cases where inflammation appears around a single tooth. This type of condition is known as localized gingivitis, and while it might seem minor, it can become serious if left untreated. Understanding how it develops, what signs to watch for, and how to treat it is essential for maintaining healthy gums and preventing further dental complications.
The idea that gingivitis can affect only one tooth may surprise some people, but dentists and researchers have documented this condition. Localized gum disease often occurs when plaque or bacteria accumulate in hard-to-reach areas, or when the structure of the mouth, dental work, or lifestyle habits create conditions for one tooth to become affected. In this article, we will explore the causes, symptoms, risks, treatment, prevention strategies, common myths, and frequently asked questions related to gingivitis in a single tooth, providing practical knowledge for anyone concerned about their oral health.
What Is Gingivitis?
Gingivitis is the medical term for inflammation of the gums caused primarily by the buildup of plaque, a sticky substance of bacteria and food particles that adheres to the teeth. Most people think of gum disease as a problem affecting multiple teeth at once, but in reality, gingivitis can sometimes present in just one tooth. This condition, referred to as localized gingivitis, is less common but still significant.
The main difference between gingivitis and periodontitis lies in the severity. Gingivitis affects only the gums and does not damage the bone supporting the teeth. Periodontitis, on the other hand, is a more severe condition that attacks the bone and tissues holding the teeth in place. Early detection of gingivitis in one tooth can prevent progression to periodontitis, tooth loss, or systemic health issues. The condition can be triggered by various factors, including poor oral hygiene, smoking, hormonal changes, medications, and even stress. Understanding what localized gingivitis looks like is crucial because it often goes unnoticed until it spreads or causes discomfort.
Can You Have Gingivitis in Only One Tooth?
Yes, it is possible to have gingivitis in one tooth, although this situation is relatively rare. Dental professionals refer to this as localized gingivitis, and it usually develops due to conditions that trap bacteria or plaque near a single tooth. Misaligned teeth, crooked teeth, or gaps can create areas where brushing and flossing are less effective, allowing plaque to accumulate. Food particles and debris can also get trapped between teeth, irritating the gums and causing inflammation localized to one area.
Poorly fitted dental work, such as crowns, fillings, bridges, or braces, can irritate the gums and lead to single-tooth gum disease. Trauma or repeated friction against one area of the gum can also result in inflammation limited to that specific tooth. Dentists have reported cases in which patients noticed slight redness, tenderness, or bleeding near a single tooth while the rest of their mouth appeared healthy. If left untreated, the condition can worsen, spreading to adjacent teeth and increasing the risk of periodontitis. Therefore, knowing that gingivitis can appear in only one tooth is critical for early intervention and long-term oral health.
Signs and Symptoms of Localized Gingivitis

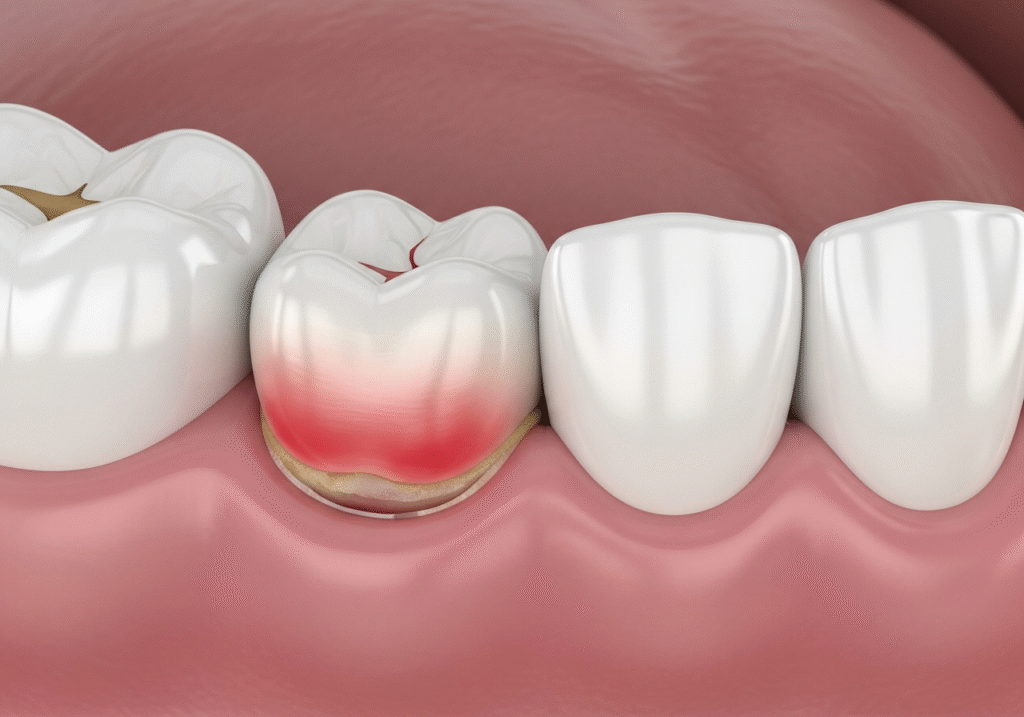
The symptoms of gingivitis in one tooth are often subtle at first, making early detection a challenge. Common signs include redness, swelling, and tenderness around the affected tooth. The gum may bleed when brushing or flossing, and some people notice a bad taste in their mouth or persistent bad breath localized near that tooth. Unlike generalized gingivitis, where symptoms are spread throughout the mouth, localized gingivitis presents itself in a single area, which can lead some people to underestimate the severity of the problem.
Patients may also experience discomfort while eating or brushing, with the affected gum feeling sore or sensitive. The area may appear shiny or darker than the surrounding healthy gum tissue. In more severe cases, pus can develop if the infection worsens, signaling the need for immediate dental intervention. Experts emphasize that even if gingivitis appears around only one tooth, it should never be ignored. Early treatment can prevent the spread of bacteria and protect other teeth and surrounding tissues.
Causes of Gingivitis in a Single Tooth
There are several reasons why gingivitis can affect just one tooth. One of the primary causes is plaque buildup in a hard-to-clean area, which may be due to misaligned teeth or uneven spacing. When a tooth does not fit well within the natural alignment of the mouth, bacteria can accumulate in areas that are difficult to reach with a toothbrush or floss. Food particles that get trapped around this tooth can worsen inflammation and lead to single-tooth gum disease.
Dental work can also be a major factor. Crowns, bridges, and fillings that do not fit perfectly can irritate the gum line and create a pocket for bacteria. Trauma, such as an injury to the mouth or excessive brushing in one area, can also trigger localized inflammation. Certain medical conditions, including diabetes, autoimmune disorders, and dry mouth caused by medications, increase the risk of gingivitis in one tooth. Research indicates that even minor plaque accumulation in a localized area can lead to gum tissue damage if left untreated. Lifestyle factors, such as smoking and poor diet, further contribute to the problem.
Risks of Ignoring Localized Gingivitis
Ignoring gingivitis in one tooth can lead to significant dental problems. If left untreated, the inflammation may spread to adjacent teeth, causing generalized gingivitis and eventually periodontitis. Periodontitis damages the bone and tissue supporting teeth, which can result in tooth loss. Patients who delay treatment for single-tooth gum disease may require more invasive dental procedures such as deep cleaning, scaling, root planing, or even tooth extraction.
Localized gum disease also carries risks beyond the mouth. Studies have linked gum infections to systemic conditions, including heart disease, diabetes, and respiratory infections. The bacteria from an untreated gum infection can enter the bloodstream, potentially affecting other organs. Dentists often warn patients that even though gingivitis may appear mild when affecting only one tooth, it is important to address the issue promptly to avoid serious complications.
Diagnosis and Treatment
Diagnosing localized gingivitis involves a dental examination, probing the gum pockets, and sometimes using X-rays to assess the surrounding bone and tissue. Dentists check for swelling, redness, bleeding, and tenderness around the affected tooth. Early diagnosis is key to preventing the condition from spreading or becoming more severe.
Treatment typically begins with professional cleaning, including scaling and polishing, to remove plaque and tartar. In some cases, dentists recommend antimicrobial mouthwash or localized antibiotics if the infection is more advanced. Home care is equally important, and patients are advised to brush twice daily, floss carefully around the affected tooth, and maintain a routine dental schedule. For individuals with dental appliances, orthodontic adjustments or reshaping of crowns and fillings may be necessary to prevent recurrence. Treatment for one tooth gingivitis is generally straightforward when caught early but can become complex if neglected for months or years.
Prevention Strategies
Preventing gingivitis in one tooth starts with consistent oral hygiene practices. Brushing twice a day with fluoride toothpaste, flossing daily, and using an antimicrobial mouthwash help keep plaque levels under control. Regular dental checkups every six months allow dentists to identify and treat early signs of gum disease before it progresses. People with crowns, bridges, or braces should pay special attention to these areas, ensuring they are cleaned thoroughly.
Avoiding smoking and limiting sugary or acidic foods reduces the risk of gum inflammation. Proper techniques, such as brushing at a 45-degree angle and gently flossing along the gum line, can prevent irritation and plaque buildup. Healthy oral habits, combined with regular professional care, are the most effective ways to avoid localized gum disease and maintain overall dental health.
Common Myths About Localized Gingivitis

Several myths surround gingivitis in one tooth. Some people believe that gum disease cannot affect just one tooth, assuming it always spreads across the mouth. However, dentists confirm that localized gum inflammation is possible and requires attention. Another common myth is that bleeding gums are normal, when in reality, it is often a sign of early gum disease. Some people also think that mouthwash alone can cure gingivitis, but without mechanical cleaning of the teeth and gums, bacteria continue to accumulate.
Dental professionals emphasize that ignoring even minor symptoms can have serious consequences. Early treatment prevents the spread of infection and protects the bone and tissue around the teeth. Understanding the truth about single-tooth gingivitis helps patients take proactive steps to protect their oral health and prevent systemic complications.
FAQs
Patients often have questions about localized gingivitis. One common question is whether it can heal on its own. While mild inflammation may temporarily improve with better oral hygiene, untreated cases generally worsen over time. Another concern is how quickly it spreads to other teeth. The timeline varies based on oral care habits, immune system health, and other medical conditions. Pain is usually mild initially but can intensify if left untreated. Bad breath or a metallic taste is common as bacteria accumulate near the affected tooth. Consulting a dentist ensures that gingivitis in one tooth is properly managed, preventing further complications.
Conclusion
In conclusion, it is entirely possible to have gingivitis in one tooth, known as localized gingivitis. While it may seem minor at first, early detection and treatment are essential to prevent the condition from spreading and causing tooth loss or systemic health issues. Maintaining consistent oral hygiene, scheduling regular dental visits, and addressing any signs of gum inflammation promptly are the best strategies for protecting your teeth. If you notice redness, swelling, or bleeding near a single tooth, do not ignore it. Timely professional care can preserve your smile and overall health.
Remember, even a single affected tooth can be the starting point of more serious dental problems. Being proactive about oral care ensures that single-tooth gum disease does not turn into a widespread and damaging condition. Take care of your gums today, and your teeth will thank you for a lifetime.
Tips for Swollen Gums and Localized Gingivitis

- Practice Gentle Brushing: Use a soft-bristled toothbrush and brush at a 45-degree angle to the gum line to remove plaque without irritating your gums. Avoid aggressive brushing.
- Floss Carefully: Slide floss gently between teeth to remove trapped food. Don’t snap or force the floss, especially near a sensitive tooth, as this can worsen swelling.
- Rinse with Saltwater: Mix half a teaspoon of salt in a glass of warm water and rinse your mouth 2–3 times a day. This helps reduce inflammation and bacteria around the affected tooth.
- Use Antimicrobial Mouthwash: An alcohol-free mouthwash can reduce bacteria and promote healing, especially when you have localized gingivitis.
- Apply a Cold Compress: For swelling or discomfort, place a cold compress on the outside of your cheek for 10–15 minutes.
- Stay Hydrated and Eat Soft Foods: Water helps wash away food particles, and soft foods reduce irritation while the gums heal.
- Avoid Tobacco and Irritants: Smoking and acidic or very sugary foods can worsen gum inflammation and slow healing.
- Schedule a Dental Checkup: Even if pain is mild or absent, a dentist can clean hard-to-reach areas and check for early infection, preventing complications.
FAQ
Why is my gum swollen around one tooth in the back?
Swelling around one tooth often happens due to plaque buildup, trapped food particles, or irritation from dental work. It can also indicate localized gingivitis or a minor infection near that tooth.
Gingivitis on one tooth
Gingivitis on one tooth occurs when bacteria and plaque irritate the gum around a single tooth. It causes redness, swelling, and sometimes bleeding, and can worsen if untreated.
How to treat a swollen gum around one tooth
Treatment involves proper oral hygiene, gently brushing and flossing, and rinsing with an antimicrobial mouthwash. If swelling persists, a dentist may perform a professional cleaning or prescribe medication.
Why is my gum swollen around one tooth no pain
Sometimes, gums can swell without pain due to early gingivitis or mild irritation. Lack of discomfort doesn’t mean it’s harmless, and early care can prevent infection.
Gum swollen around one tooth overnight
Sudden swelling overnight can result from trapped food particles, minor trauma, or a developing infection. Rinsing with salt water can reduce irritation while monitoring for worsening symptoms.
What is the fastest way to heal swollen gums
The quickest relief comes from warm saltwater rinses, proper brushing and flossing, and avoiding irritants like hard foods or smoking. Persistent swelling requires professional dental care.
Gum swollen around one tooth after flossing
Flossing can sometimes irritate the gum if done too forcefully, causing temporary swelling or bleeding. Using gentle, correct technique usually prevents this issue.
Swollen gums treatment at home
At-home care includes saltwater rinses, cold compresses for comfort, maintaining oral hygiene, and using antimicrobial mouthwash. Persistent swelling or pain should be evaluated by a dentist.